Research
Our research to conceive new cardiovascular monitoring paradigms integrates (1) physiology in the form of mathematical or qualitative models, (2) data analytics including signal processing, parameter estimation, system identification, and machine learning, and (3) sensors such as those already in clinical use or in mobile devices, emerging wearables, and multi-transducer systems. We also seek to validate the integrated concepts in laboratory subjects and patients under diverse physiologic conditions. In this way, our multi-disciplinary research may ultimately help in reaching the full potential of cardiovascular health tech. Our specific areas of contribution include the following.
Advanced Blood Pressure Measurement: Cuff blood pressure measurement devices have been instrumental in our fight against hypertension – the number one cause of disability-adjusted life years lost worldwide. However, cuff devices are not readily available, especially in low resource settings, and cumbersome to use. Due in part to these limitations, hypertension awareness and control rates are low. Furthermore, cuff devices often do not provide accurate enough information, so a significant fraction of patients end up being misclassified in terms of hypertension stage. We have developed various concepts to advance blood pressure measurement in terms of accuracy and convenience.
Hemodynamic Monitoring by Blood Pressure Waveform Analysis: Blood pressure waveforms are measured in millions of surgery and intensive care patients each year. However, other difficult-to-measure hemodynamic variables such as cardiac output and cardiac filling pressures are needed to determine the etiology of frequent hypotension and guide therapy. We have developed a number of methods to compute central hemodynamic variables of proven clinical value from more readily available blood pressure waveforms. In this way, hemodynamic monitoring may become automated and less invasive without requiring any instrumentation beyond what is already in use.
Probing Neural Cardiovascular Regulation by System Identification: The baroreflex and other neural cardiovascular regulatory mechanisms maintain blood pressures through feedback and control so as to protect blood flow to the vital organs in the face of exogenous perturbations such as exercise and postural changes. In contrast to longstanding beliefs, recent evidence shows that the baroreflex can contribute to long-term blood pressure maintenance. Hence, neural cardiovascular regulatory mechanisms could possibly play a causative or protective role in hypertension and heart failure. We have developed various techniques to quantitatively probe and thus elucidate these increasingly important mechanisms by applying system identification analysis to beat-to-beat fluctuations in multiple cardio-respiratory signals.
Cuff-less blood pressure (BP) measurement: The state-of-the-art in the field including pulse transit time (PTT) and photoplethysmography (PPG) waveform analysis is summarized through reviews/book chapters/editorials.
Mukkamala R, Yavarimanesh M, Natarajan K, Hahn JO, Kyriakoulis KG, Avolio AP, Stergiou GS. Evaluation of the accuracy of cuffless blood pressure measurement devices: challenges and proposals. Hypertension,78(5):1161-1167, 2021
Mukkamala R, Hahn JO, Chandrasekhar A. Photoplethysmography in Non-Invasive Blood Pressure Monitoring. Photoplethysmography.Eds. Kyriacou P, Allen J. London: Academic Press, pp. 359-400, 2022.
Natarajan K, Yavarimanesh M, Weng W, Mukkamala R. Camera-Based Blood Pressure Monitoring. Contactless Vital Signs Monitoring.Eds. Wang W, Wang X. London: Academic Press, 117-148, 2022.
Mukkamala R. Blood pressure with a click of a camera? Circulation: Cardiovascular Imaging, 12(8):e009531, 2019.
Mukkamala R, Hahn JO. Calibration of Pulse Transit Time-Based Blood Pressure Monitors. The Handbook of Cuffless Blood Pressure Monitoring. Eds. Sola J, Delgado-Gonzalo R. New York: Springer, 163-190, 2019.
Mukkamala R, Hahn JO, Inan OT, Mestha LK, Kim CS, Toreyin H, Kyal S. Toward ubiquitous blood pressure monitoring via pulse transit time: Theory and practice. IEEE Transactions on Biomedical Engineering, 62(8):1879-1901, 2015.

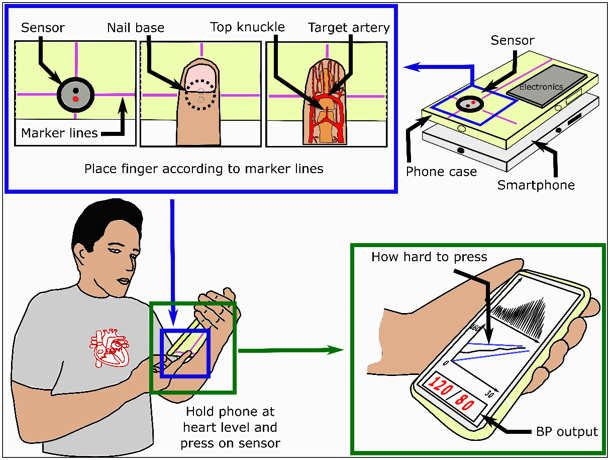
Cuff-less BP measurement: The oscillometric finger pressing method permits cuff-less and calibration-free BP monitoring via a smartphone.
Chandrasekhar A, Natarajan K, Yavarimanesh M, Mukkamala R. An iPhone application for blood pressure monitoring via the oscillometric finger pressing method. Scientific Reports, 8(1):13136, 2018.
Chandrasekhar A, Kim CS, Naji M, Natarajan K, Hahn JO, Mukkamala R. Smartphone-based blood pressure monitoring via the oscillometric finger pressing method. Science Translational Medicine, 10(431):eaap8674, 2018
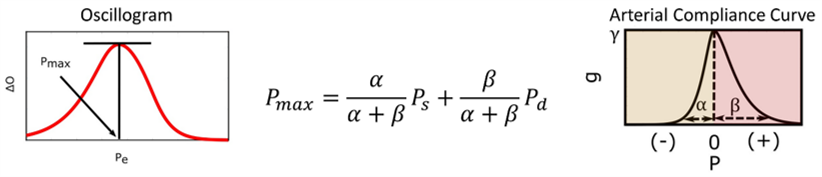
Oscillometric BP measurement: The external pressure at which the oscillogram is maximal (Pmax) denotes a weighted average of systolic and diastolic BP (Ps and Pd) rather than commonly believed mean blood pressure.
Chandrasekhar A, Yavarimanesh M, Hahn JO, Mukkamala R. Formulas for explaining popular oscillometric blood pressure estimation algorithms. Frontiers in Physiology, 10:1415, 2019.
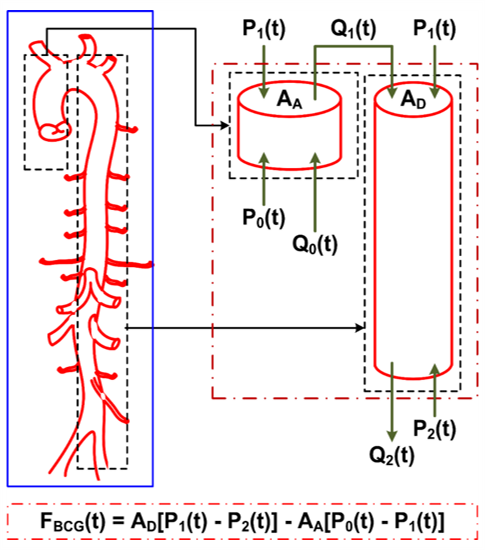
Ballistocardiography: The mechanism of the ballistocardiogram (BCG) waves is the difference in BP gradients in the ascending and descending aorta.
Kim CS, Ober SL, McMurtry MS, Finegan BA, Inan OT, Mukkamala R*, Hahn JO*. Ballistocardiogram: mechanism and potential for unobtrusive cardiovascular health monitoring. Scientific Reports, 6:31297, 2016.
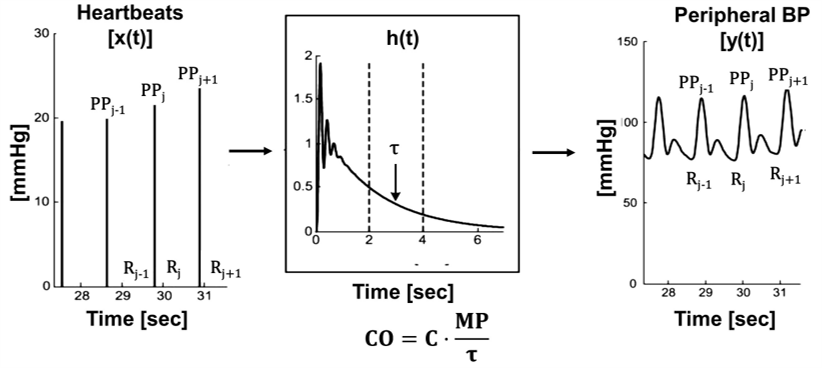
BP waveform analysis: Multi-beat analysis for computing cardiac output (CO) from a peripheral arterial BP waveform circumvents confounding arterial wave reflection.
Mukkamala R, Kohl BA, Mahajan A. Comparison of accuracy of two uncalibrated pulse contour cardiac output monitors in off-pump coronary artery bypass surgery patients using pulmonary artery catheter-thermodilution as a reference. BMC Anesthesiol. 2021 Jul 10;21(1):189.
Zhang G, Mukkamala R. Continuous and minimally invasive cardiac output monitoring by long time interval analysis of a radial arterial blood pressure waveform: assessment using a large, public intensive care unit patient database. British Journal of Anaesthesia, 109(3):339-344, 2012.
Reisner AT, Xu D, Ryan KL, Convertino VA, Rickards CA, Mukkamala R. Monitoring non-invasive cardiac output and stroke volume during experimental human hypovolemia and resuscitation. British Journal of Anaesthesia, 106(1):23-30, 2011.
Lu Z, Mukkamala R. Continuous cardiac output monitoring in humans by invasive and non-invasive peripheral blood pressure waveform analysis. Journal of Applied Physiology, 101(2):598-608, 2006.
Mukkamala R, Reisner AT, Hojman HM, Mark RG, Cohen RJ. Continuous cardiac output monitoring by peripheral blood pressure waveform analysis. IEEE Transactions on Biomedical Engineering, 53(3):459-467, 2006.
BP waveform analysis: Left ventricular ejection fraction can be computed from arterial waveforms.
Swamy G, Kuiper J, Gudur MSR, Olivier NB, Mukkamala R. Continuous left ventricular ejection fraction monitoring by aortic pressure waveform analysis. Annals of Biomedical Engineering, 37(6):1055-1068, 2009.
Mukkamala R, Kuiper J, Sala-Mercado JA, Hammond RL, Kim J, Stephenson LW, O'Leary DS. Continuous left ventricular ejection fraction monitoring by central aortic pressure waveform analysis. Proceedings of the 28th Annual Conference of the IEEE Engineering in Medicine and Biology Society, 1:620-623, 2006.
Probing neural cardiovascular regulation: The nonlinear kernels characterizing the open-loop baroreflex system relating carotid sinus BP to arterial BP are diagonal in structure.
Moslehpour M*, Kawada T*, Sunagawa K, Sugimachi M, Mukkamala R. Nonlinear identification of the total baroreflex arc: higher-order nonlinearity. American Journal of Physiology, 311(6):R994-R1003, 2016.
Moslehpour M, Kawada T, Sunagawa K, Sugimachi M, Mukkamala R. Nonlinear identification of the total baroreflex arc: chronic hypertension model. American Journal of Physiology, 310(9):R819-R827, 2016.
Moslehpour M, Kawada T, Sunagawa K, Sugimachi M, Mukkamala R. Nonlinear identification of the total baroreflex arc. American Journal of Physiology, 309(12):R1479-R1489, 2015.